Medical Information
Medical Treatment & Hospitalization
Refused treatment in ED including oxygen and monoclonal antibodies. Once admitted, isolated from family, disregarding effects of anxiety causing decline in respiratory drive and need to intubation for ventilation. Administered Remdesivir protocol without adequately informed consent. Later transferred to facility so wife could stay with patient.
Activism & Follow-up
Watch & Share The Interview
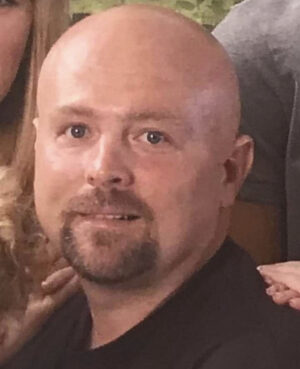
Written by Renee Rutherford(Wife)
I don’t even know how to begin telling this story, the most horrific story I could have never imagined. I guess it makes since that you know a little about me. I am a master’s prepared nurse and was a student in a nurse practitioner, doctorate program when my husband got sick. I have worked in many areas in the nursing field over nearly two decades, from acute care, emergency, home care, hospice, and administration. At the start of the coronavirus pandemic (or plandemic), I had been away from bedside nursing for a few years. I was working with a large hospital system in the patient finacial services department where I conducted medical reviews for financial assistance (AKA charity care). In that role, COVID protocols had no direct impact on me aside from allowing me to work from home. I attended meetings virtually, and communicated with co-workers and colleges via telephone, instant message, or email. Treatment protocols for COVID had no impact on my work, so I did not delve into the details.
The plandemic only began to affect me personally when the hospital system mandated the COVID vaccines for all employees. It didn’t matter that I worked from home with no exposure to other hospital employees or patients. Like many, I had not chosen to get the vaccines after they were introduced because I recognized they were experimental, and I had no risk factors for which participating in such an experiment might be beneficial. Due the mandate, I had until August 2021 to submit a request for exemption or until October to get the vaccines. I knew exemptions were not likely to be granted, I would be subject to required weekly testing, and would not be eligible for raises or bonuses without I took the vaccines. Still hesitant, I reached out to my Facebook friends and asked them to share their experiences if they had received the vaccine. Most who had received the vaccines reported no side effects or only mild side effects of arm soreness, low grade fever, and/or mild cold symptoms that lasted only a day or two. Others reported having had COVID with symptoms that ranged from minor to shortness of breath. Still others reported ongoing symptoms for months following a COVID diagnosis. Finally, I asked my FB friends for prayer for God’s leadership and guidance in my life regarding my role in medical freedom and vaccine mandates for myself and others.
After much hesitation I went to employee health and got the Johnson & Johnson vaccine on August 26th. I chose the Johnson & Johnson vaccine because, at that time, it was only one shot, and didn’t contain the experimental mRNA component the Pfizer and Moderna vaccines did. Later that afternoon, when my active, healthy, strong husband learned I had gotten the vaccine, he decided he wanted to get the vaccine too. He also wanted to get the Johnson & Johnson vaccine. He said he was afraid if he had a reaction to one shot, he would not go back to get a second one, but we were not able to find a location administering the Johnson & Johnson vaccine that evening. Not being familiar with any studies that might have helped in choosing (or not) the Pfizer or Moderna vaccine, he decided to get the first Pfizer vaccine at the Walmart Pharmacy. He received the first Pfizer vaccine on August 26th. The following day we headed out with our brand-new camper, we had purchased as a 30th wedding anniversary gift for ourselves, to a local campground for a short weekend trip. My husband reported minor soreness in his arm the following day, but it didn’t slow him down or alter his activity.
Our daughter, her boyfriend, and infant son joined us on our camping trip on the afternoon of August 28th and spent the night in our camper. On the morning of August 29th, our infant grandson started running a fever, so my daughter and her boyfriend took him home. I later learned my daughter’s boyfriend was complaining of a headache and minor congestion when they joined us on the 28th. My grandson went to the doctor on the 30th and was negative for flu and RSV. He was not tested for COVID. My daughter then started having a headache and fever on the 31st. Because she had fever, her employer required she be tested for COVID before she could return to work. She received a positive COVID result on September 1st. On the same day, my husband began running a low-grade fever, so we knew he likely had COVID as well, but he continued to work in the field on a tractor (alone, without exposing others) for the next two days. During that time, he started taking vitamin D, vitamin C, Mucinex for congestion, and alternating Tylenol and Ibuprofen for fever. On Saturday, September 4th he continued to struggle to get his fever down and his congestion and fatigue worsened so he called the on-call provider who only recommended the Tylenol, Ibuprofen, and vitamins he was already taking. The following day, his fever remained elevated even with medicine and he developed ear pain in addition to the congestion, so he called the on-call provider again to see if she would treat him due to ongoing and worsening symptoms. She told him he could take Mucinex (which he was already taking) and start taking a baby aspirin daily; otherwise, he would need to be tested for COVID before she could give him anything else for his symptoms. The following morning, he reported feeling short of breath and allowed me to listen to his lungs which were clear with good air movement. I hunted an old pulse-oximeter, replaced the battery and checked his oxygen levels with were in the mid to upper 80’s, so he agreed to go to the hospital although he knew he would likely have to go in alone, because the hospitals were not allowing visitors since the pandemic began.
Because he was feeling so bad, once we got to the emergency department (ED), I left my husband in the car and went to the ED door to see if they would allow me to check him in and call him once they had a room ready. By doing so, clerical staff and those in ED waiting would have less exposure to him; however, I was told I was not allowed to come in, but he would have to come in and register himself. While in the ED he text me that his oxygen levels were 83-85 at rest but they did not give him any oxygen. He said the doctor told him the 80s were the new 90s with COVID and that oxygen would not help him. His COVID test was positive, chest x-ray was positive for COVID pneumonia, no labs were drawn, and he was discharged with instructions to get an antibody infusion when a clinic in a neighboring community called with an appointment and a prescription for Zofran, a medication for nausea (I have no idea why that would be the one prescription they gave him). Feeling very discouraged and anxious, we went home to try to treat him the best way we knew how until we could get the antibody therapy. He tried to walk around in the driveway but was so weak and short of breath he had to stop and rest after only a few steps. I called the clinic where they recommended, he get the antibody therapy and got a message that they would be closed until Tuesday, September 8th so I called a neighboring hospital I knew had been giving antibody infusions. Their infusion clinic was also closed, and I was instructed to call back the next day. That night, I slept with my hand on his back, so I knew he was still breathing.
The following morning, September 7th, I called the infusion clinic as soon as they opened and was told I could bring him right on. When we got to the clinic his oxygen levels were in the mid to low 70’s. They told him his oxygen levels were too low to receive the antibody therapy and would have to go to their ED. Again, I was not allowed to go in with him. Once in the ED he texted me and told me his oxygen levels were in the 90s after they put oxygen on him but it was “blowing hard”. They had put him on high-flow oxygen. He then texted me and said they were going to admit him but would not allow me to come in because of other COVID patients. Later he texted me and said they were starting Dexamethasone and Remdesivir. Although, the thoughts of him receiving an experimental drug was scary, I knew he had to be treated with something or he was likely to die. I had to trust that the nurses and therapists would monitor him closely and intervene as needed. Needless to say, I was scared out of my mind and unable to focus on much other than fear.
At 4:20 pm he texted me and said he was getting his first dose of Remdesivir. At 5:20 he texted and said he was doing okay, but at 7:46 pm the respiratory therapist texted from my husband’s phone and said they had to place him on bipap at 18/12 and 100% to get his oxygen level to 91%. He said he was “rounding on him and he was on heated high flow doing well, but then just dropped out of the blue”. Unfortunately, no one thought to consider the possibility of a medication reaction and neither did I. At that point I was not able to think clearly. I had slept very little over the last few days and was distraught that I was not allowed to be with my husband as he was fighting for his life. Had I have been able to be with him, my mind may have been somewhat clearer, so I could have been a better critical thinker, but knowing my husband was alone fighting for his life and I could not be there to help was crippling.
Because he was put on bipap, he would have to be admitted to ICU; however, there were no ICU beds, so he had to stay in the ED until late the next day. While he was in the ED, the nurse took an ipad on a stand in his room so I could facetime with him, but once he was admitted to ICU, I had no contact because he was too weak to hold his phone to talk or text me. I finally recalled that a friend and former co-worker had gone to work for the hospital my husband was in, so I messaged her to see if there was anything she could do to get me in to see my husband, and she did. She said she had talked with the ICU manager and house supervisor, and they had agreed to allow me to visit. I finally got to see him the evening of the 9th.
He remained on bipap while I was visiting with him and his oxygen levels stayed in the 90’s as long as the bipap mask was on, but he was noticeably fatigued so when he was able to rest, I just sat by him quietly and let him rest. During my visit, the nurse told me they had to give him morphine and Ativan for agitation the night prior, but he did not tolerate it well. I explained that he had never been on medications other a medicine for blood pressure control. When he would fall asleep, he would sometimes get startled by the noises in the hospital and his first reaction was to pull his bipap mask off which would result in his oxygen levels dropping and the nurses having to come in his room to put the mask back on. You must understand, this man was always a fierce protector. If ever something went wrong, he would always handle whatever the problem was. He would guard his family from all harm at any cost. That was his nature. While I was there, I was able to gently place my hand on his arm and remind him he was in the hospital, and he would relax without pulling at the mask.
A little after 9:00 pm a lady I later learned was the ICU manager came in the room and told me visiting hours were over and I would need to leave soon. Then she left the room. As I sat there with my husband, I noticed he continued to startle easily but was calmed by my presence. Being anxious in a healthcare setting was not something that was new for my husband. He had avoided going to the doctor for most of our married lives and only recently had he shared his fear of doctors with me. Although I had been told I would have to leave, I just couldn’t, so I didn’t. Then the charge nurse came in and told me it was time for me to leave. I explained to her that my being there was helping my husband stay calm and keep the bipap mask on. She said it was not her decision to allow me to stay but would discuss it with the house supervisor. The house supervisor then came into the room and told me it was the hospital protocol that no one could stay with patients with COVID and that I would have to leave. I again explained that my being there was keeping him calm and his bipap mask on. I explained that if I were to leave, he would get anxious which would cause him to pull at his bipap mask and in order for them to keep his mask on they would have to give him antianxiety medications which he did not tolerate and would suppress his respiratory drive and cause him to require intubation and to be placed on a ventilator. I pleaded with her to let me stay. I explained that I too had managed an ICU and understood hospital policy but that policies should ALWAYS allow for the best care of the patient and in my husband’s case, it was best for him for me to be there. She continued to tell me she had to follow policy. At one point she even said “all these other patients need their families too. It wouldn’t be fair to them if we let you stay”. At that point I couldn’t believe what I was hearing and told her that if she did not advocate for what was best for her patients, she was failing them. She finally said “okay, I’ll call administration and see what they say”. When she returned to the room, she motioned for me to come out of the room, so I met her at the door. I knew they were not going to let me stay. They would have escorted me out if I didn’t go. She said she talked with administration and that I would have to leave, so I returned to my husband’s side and told him I was going to have to leave. He said, “but you’ll be back by five, won’t you?” When I told him I didn’t know if they were going to let me come back, he got upset. I asked him to please try to stay calm, told him I loved him and turned and walked away just after midnight. I cried all the way home.
About an hour and 20 minutes after leaving my husband’s hospital room and just after falling to sleep, I received a call from the doctor. She said they had already been working with my husband for over an hour, they had given him every medicine they could give him, and his oxygen levels were in the 50s. She said they needed to intubate him, but he insisted they call me first. I was beyond shocked and angry that they had made me leave and even more shocked and angry that they had not called me back before he had declined so significantly. I asked if I could come back to which she replied, “you can, but you need to understand, he will probably code before you can get here”. In tears, I said, “what do you want me to do?” She said, “I just need to know if we can put him on the ventilator”. I screamed, “you are killing my husband”. Again, she said, “his oxygen levels are in the 50’s. Do you want us to intubate him?” I felt I had no other options at that point and told them “Yes”. I then heard her ask my husband, “what do you want me to tell your wife?” to which I heard him say “tell her I’m trying” and she disconnected the call. Within 30 minutes she called back and said he was on the ventilator but that his lung had collapsed, and they were having to put a chest tube in.
The next morning, I called one of the hospitalists at my local hospital where I had worked much of my career and asked them if they could take him as a transfer. He graciously told me he expected to have a bed available in the ICU the next day. He told me to have the doctor at the hospital he was in to call him, and they would work out the transfer. He was transferred to our local hospital the following evening; September 11th, and I was finally allowed to stay with him. When I walked into his room, I noticed his T waves on the cardiac monitor were inverted, but no one could tell me when that happened. I have since learned he had inverted “T’s” on his initial EKG in the ED. They told me his echocardiogram looked good and showed he had a strong heart. In many ways it did, but I later learned his echocardiogram showed a significantly enlarged right atrium with completely normal function of all valves.
Although I am grateful to the doctors and nurses for allowing me to stay, still there were several medical errors made that only worsened his critical condition. He was given blood pressure medicine when his blood pressure was already low resulting in having to give him pressors to bring it back up. His oxygen was weaned based on faulty pulse oximeter readings resulting in critically low blood oxygen levels. The emergent nature of a second collapsed lung was not recognized for several minutes, delaying surgical intervention. After 45 days in the hospital and 42 days on a ventilator, my husband died on his 50th birthday.
Unfortunately, I will likely never know the exact cause of my husband’s death, but I know, whatever, the ‘cause’, policies lead to his demise. Did the Pfizer vaccine play a role? – likely. Did the administration of remdesivir play a role? – likely. Did medical errors play a role? – likely. Did withholding of early treatment play a role? – most certainly. Did segregation and solitary confinement play a role? – most certainly.
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please contact us at email@chbmp.org.