
Medical Information
Medical Treatment & Hospitalization
Poorly except for one RN who really communicated with us and whom my husband liked.
Activism & Follow-up
Watch & Share The Interview
Written by Debbie Gregory (Spouse)
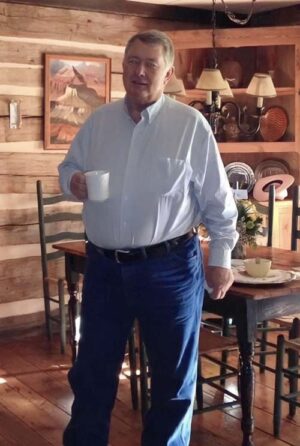
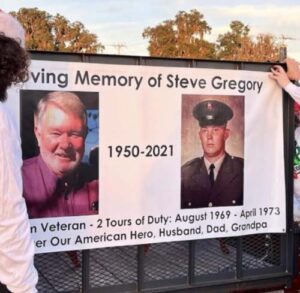
My husband Steve Gregory died on September 13th 2021, at the Malcolm Randall VA hospital in Gainesville, Florida. He was 70 years of age, just short of 71 years. His birthday is in October. Steve’s upbringing was on cattle ranches, and he loved all things about the country life – a true cowboy.
He served his country during the Vietnam War. He did 2 tours of duty over there, and we met soon after his return, stateside, on good old Main Street, USA. He wanted to meet me and I wanted to drive his car! Lol
In June of 2021 we had just celebrated 47 years of marriage. We have 3 children, 12 grandchildren, plus 2 great grandkids, but sadly he wasn’t here to meet his latest great grandchild, who was named Stephen, in honor of his Great Grandpa.
I hate the joy that’s been robbed from our family!! We’ve always been all about family, and my husband loved nothing better than to back up into the yard in his semi and see all those kids playing in the pool, and so excited to see their grandpa!
Steve drove truck and would be gone almost a month at a time, so anytime he came home, it was a celebration and almost always, the kids would all spend the night. Steve loved getting up and seeing the living room full of sleeping kids and smelling breakfast cooking! My grands loved breakfast with grandpa – sausage-bacon gravy, biscuits and eggs.
Most of the kids are grown now but we would still gather when he came home and vacation together. Sharing this small part of our lives just to try, in a small way, to emphasize the hole that’s been left in our hearts without him being here!! Death is a part of life, but for someone to be taken in this way is so beyond to be touched by evil that I guess it just something that’s hard to believe would happen in our American hospitals. Especially in a hospital that represents a veteran who stood in the gap during wartime to protect so many who walk those corridors!!
Now to tell my husband’s story and what he endured at the hands of those who took an oath to do no harm – to actually use those hands to try and do all to help heal.
In August of 2021, my husband had come home, and we were having the family over to enjoy a visit from our son who was visiting from Virginia. During that week, I began to feel exceptionally tired, exhausted really, but I didn’t stop; too much to do. On the 12th, I realized I had no taste or smell. I had hydroxychloroquine, zinc, and vitamin C on hand, and immediately I started my husband and myself taking these. What I didn’t realize, at the time, was I think my husband needed a larger dosage for it to be effective.
On the 16th, I tested positive for COVID-19, and my husband was tested on the 19th, which was positive also. The middle of the night on the 20th, Steve wanted to go to the ER at the VA but we talked about it ( we were aware of remdesivir and ventilation), and he decided to wait. Steve slept in the recliner sitting up which seemed to help.
The next morning the 21st, my sister who was very concerned about us had called and had a VA nurse on the call. The nurse asked for Steve’s oxygen levels which were at 88. She immediately said he needed to go to the ER, and that’s all it took for my husband to get dress to go.
On the way, I kept asking Steve, “Are you sure?” He would just nod his head “yes,” plus I asked him more than once should I give our oldest son a call, but he would just nod “no.” I so wish I had called my son! Things might of gone differently!!
We arrived at the hospital, and they wouldn’t let me go in with him. I rubbed his arm as he went in I so wished I’d hugged him but… He called me later when he got to a room. They had him on supplemental oxygen and he felt better. He also told me of a nurse or so he thought she was a nurse. He called her the Gestapo nurse. It was actually a Dr. Neal, and she had told him, “If you don’t get up and walk 3-4 times a day, plus shower, you will die in here!” He didn’t like her being so blunt, I guess, but in hindsight, she was trying to help him, I guess.
The doctor’s hospital notes said he needed to mobilize ambulate and shower. I talked with Dr. Neal later that day, and she told me the same, plus I asked her about remdesivir and her words were “It doesn’t help.” Yet, looking back on his hospital notes, they started him that first night on remdesivir. He had 5 doses of it and 10 days of dexamethasone.
On his admittance, it’s noted that Steve stated, “No remdesivir and No ventilation,” plus he signed a DNR. It’s also stated that Steve was not vaccinated.
Next morning the 22nd, Steve got up and walked and took a shower which I had urged him to do. When I talked to him afterwards he was upset with me. He told me I got him in big trouble!! The nurses were not happy with him, said he made a big mess. The RN Christine forbid him to get up anymore. I talked with her and said the doctor had said he needed to do those things, but she said Steve could fall and break a hip. So I asked, why can’t someone help him, but her response was they we’re too busy!
Next day the 23rd, a different doctor, and he had same instructions for Steve. I told him the nurses would not let Steve get up. He said he would talk to them.
At 9 a.m. the next morning the 24th, I called Steve (He had his cell phone with him, and that’s how we were talking.) RN Christine, was in the room with him. She gave me an update, and I told Steve I’d call back soon. At 9:24, I got 2 texts from Steve’s phone saying, “Call me.” 🤙 I thought that’s strange, he’s never used that emoji before. I tried over and over to call him but I couldn’t get through. I told him I’m calling, but I can’t get through. He never replied, so at 10 a.m., I called on the hospital phone. It’s noted in hospital notes “wife called an hour after last update.” 2 p.m., I called again and again noted in notes “Respiratory therapist: wife called questions answered.”
I had an appointment in town that afternoon and while I was there, RN Christine, called to give an update. I expressed to her my concern about Steve not being able to mobilize even though it was the doctors’ orders, and her response was, “she wished doctors wouldn’t say those things.”
I asked my daughter to try calling her dad, and she got through to him, so I suspected I had been blocked. Not only did my husband not know how to block someone, he didn’t know how to unblock someone!
The next morning the 25th, I called Steve’s room again on the hospital phone, and a nurse helped me with Steve’s phone, and sure enough my number had been blocked! I have no proof, but I believe that RN Christine, blocked my number because she was in the room with Steve during the timespan when I got the weird texts.
This same day, the 25th, Steve began to throw up coffee ground emesis while also trying to insert an NG tube; 300cc of red blood came up. They called about needing to transfer Steve to the VA in Gainesville, Florida, because Lake City VA, didn’t have a blood bank.
A couple of days after Steve was admitted, I remembered I could access his labs and doctor notes. In doing this I saw where he had signed a DNR. I was shocked, and asked him to rescind that DNR especially in light of not knowing what might take place. I didn’t want to lose him.
That afternoon they transferred Steve. In the notes of his arrival in Gainesville, it’s noted that Steve’s oxygen was down to 82% and that he was immediately placed on ICU ventilator. In the records it states:
O2 tank empty
Bag not inflated
SPO2 was initially at 82% from transport
Steve and I were glad he was in Gainesville; thought he’d get better care than what was taking place in Lake City. At 4 a.m. on the 26th, I received a call that Steve needed emergency surgery for a gastric perforation. I was told without it he would die, but he might not make it through surgery either because of the COVID-19, also that Steve would be intubated. In hospital notes it states:
“GI Tract Perforation after receiving Tocilizumab Treatment halted”
Steve made it through surgery, and for the next 9 days, he was on a ventilator. On the 28th Steve was awake and alert. Squeezed the RN’s hand. We were so happy. During those first few days, I would call and the attending, RN Neal, would help me to FaceTime my husband on his cell phone. I added my kids on the calls so we could talk to Steve. He could express himself through blinks and nods. RN Neal became someone that my husband, our kids and I appreciated so much!
At some point, we were able to talk to Steve by a chaplain taking an iPad to Steve’s room. So daily, I would get updates and talk to Steve. Everything seemed to be going good, and after 9, days Steve was off the ventilator. Steve was extubated on 9/3. When I talked with doctors, they were always telling me how sick Steve was, but to us he seemed to be improving each day. One chaplain expressed how it put a smile on his face every time he saw Steve, cause he was always sitting up alert and awake. He was the only one on that floor who was.
One morning Steve was in a lot of pain but couldn’t get any help. When the morning shift got there, RN Neal was his nurse. The overnight nurse never emptied Steve’s catheter bag, and it was backing up causing pain! In Conversation with RN Neal, he said, “He was a veteran also and that he was trying to change the culture there – he said, they don’t care enough.”
My husband began to express how much he wanted water. I would talk to nurses as to why couldn’t he have water. They said, “He might get chocked.” Still, we pressed them to at least to give him a sponge stick to suck on. On one particular call to Steve a nurse gave him a sponge stick with water. It was so upsetting to see Steve sucking on that stick so feverishly and the wild look in his eyes. Even though we were talking to him he wasn’t responding. It was so disturbing! I have a picture I took of him and it was one of those live pictures. He opens his eyes and says, “They think they ain’t got no water.” He told us he would watch them sitting at their station drinking out of their big cups. It was tormenting to him!! The picture I took was on 9/7 which was 5 days after being taken off ventilator. 5 days of being aware of his thirst!!
In his records, I saw where his WBC had gone up so I was telling the doctor about my concerns of infection setting in and starting antibiotics. Her response was until they knew what to treat they couldn’t start any. In his records on 9/9 it was seen in scans that were ordered:
possibility of 2 abscesses communicated to Dr. Younis
In notes, they were looking for MRSA
It states there were 2 Seromas (fluid filled pockets)
In his gastric perforation surgery notes: once the defect was closed, we attempted to pass a Dobhoff tube.
But they couldn’t get it past the pylorus so it was not placed. Was that tube for drainage to prevent infection?? Dr. Younis, even though she was aware of these findings, she didn’t start Steve on antibiotics until 9/11. They started Steve on 2 drugs used as a last resort for MRSA – Vancomycin and cefepim.
During this same period of time, RN Neal was growing concerned about Steve. Steve was becoming lethargic. He urged me to talk doctor about changing his NG tube that had been placed in Steve’s nose. Steve was experiencing a lot of pain. His nose was split from the NG tube. RN Neal said it could be replaced with a Dobhoff tube, and it would be more comfortable. An NG tube is only suppose to be placed in nose no longer than 14 days. It had now been 17 days. Was this the source of infection??
I had begun to urge doctors to let me come be with Steve. The 20-21 days required for isolation was past. Steve needed comfort from me. The doctor I had spoken too agreed. He said Steve would need to be tested again and the infectious doctors would have to approve it. Steve was tested. The COVID-19 test was negative. I could come on Sunday the 12th. Then on Saturday, I was told that the infectious doctors said I couldn’t come on Sunday because Steve had bacterial pneumonia, and I would have to wait for that to clear. I had pretty much made up my mind I was going on Monday anyway!
On Monday morning, I called to get an update on Steve and the nurse told me they might have to vent him again cause he was having trouble breathing. Not long after, I received a call from my husband’s phone. A Dr Gomez was on the line telling me they preparing to vent Steve. She was asking permission if after 2 weeks if Steve was still on ventilator could they intubate him thru his throat, and we said, “yes.” After that question, she began to tell us that Steve could go into cardiac arrest, and we should let him go peacefully. I told her, “No, resuscitate.” But again, she just kept pressing that it would be better for him to let him go peacefully! Then she started talking about how painful CPR can be. It breaks his ribs! I told her, “Resuscitate.” Again, she repeated herself, and how much better for Steve it would be to let him go peacefully.
I told her, “I’d know what to do if it came to that.” I added, “My husband rescinded his DNR, so what does that tell you!!” Finally I said, “Steve, what do you want?” and he said loudly, “I WANT TO LIVE.” I said, “You heard him!!”
When she finally stopped, I couldn’t believe this, that my husband was hearing this heated conversation between us. She was relentless! She knew what was about to happen.
An hour later, I received a call from her, and Steve had gone into cardiac arrest. They had performed CPR, but she said it would happen again. Then she asked how far was I from hospital. I told her thirty minutes. “I’m coming.” I responded. She said again, “Let him go peacefully.” I said, “No, resuscitate. I’m on my way.” On the way, she called again said, “It had happened again.” I told her I’m 15 minutes out.
When we arrived, they were working on Steve again. The room full of people. They suited me up to go in. I began to talk to my husband and pray over him. I so wanted him to live! They let my son in also, and we prayed, held Steve’s hand. At one point his oxygen levels started going up, and we thought for a moment he’s going to make it. A tear fell down my husband’s cheek. Eventually, it was over and they pronounced him dead. We stayed in the room for awhile, saying goodbye, telling Steve how much we loved him. Two nurses or not sure who they were, stayed in room with us. Before we left room, one of them began to ask us if we were going to get an autopsy? Said they do them there. Out in the hall, and again he is talking to us about getting an autopsy. He said something to the others behind nurses station about hospital doing the autopsy. They didn’t seem to like him saying that.
He directed us downstairs to some checkout station. I asked there about autopsy and was told the hospital wouldn’t do one on a COVID-19 patient. I wish I had pursued an autopsy, but I guess I just got swept up in the shock of it all-making funeral plans.
One thing in the hospital records that they never told me was: 8/26 day of surgery, it was reported on radiology notes: No abdominal aortic aneurysm present
8/30 (4 days after surgery) noted in radiology report: Abdominal aortic aneurysm present.
It was noted again in other radiology reports, but not a word to me about it!! Why didn’t they tell me and address this??? Why because, in my opinion, they knew their plan for him.
On Steve’s death certificate it states: Cause of Death: Perforated Gastric Ulcer, COVID-19 Pneumonia
The truth of what happened to our loved ones, I pray, is known across this world someday!!
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please contact us at email@chbmp.org.