Medical Information
Medical Treatment & Hospitalization
We were not allowed to stay in ER and sent home. They admitted him and while we could see him. I asked for multiple drugs or treatments. I was told outpatient only for monoclonal antibodies. Baricitinib was not available in our area. Doctor laughed when I asked for Ivermectin. Told he was given Remdesivir, and was told nothing about the drug itself. Told he was doing great and expected to go home in the next few days. The doctor never consulted with me prior to Leroy’s admission to ICU. My husband called and told me he was being moved to ICU so they could monitor him better. We do not know how he was treated on a daily basis, as we were not allowed to see him until they phoned to say we needed to have an end of life discussion. The physician stated Leroy had developed Fibro Prolific Acute Respiratory Distress Syndrome. That his lung tissue was like Papier-mâché. After the doctor left, the nurse came in and Leroy attempted to ask her if he could sit up. She told him, “No.” They had tried that earlier and he had turned blue. He then commented he just wanted to talk with his wife. She then stated the only reason I was there was because he was dying. You could see his face turn white. I had been told by the case worker that our children were to come the next day and what was that to look like? All of us at once or individually? She stated that no one was allowed.
Activism & Follow-up
Watch & Share The Interview
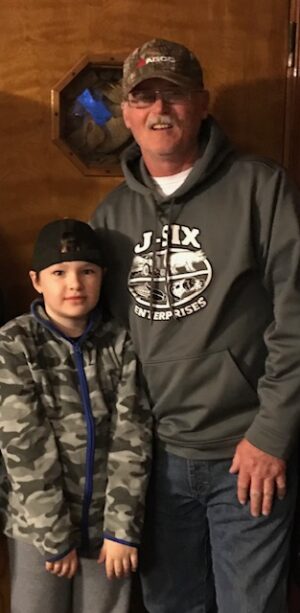
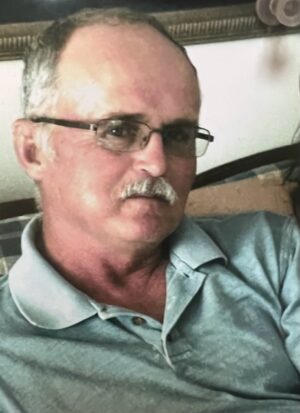
Written by Sheryl E Garland(Widow - Spouse)
After several days with Covid, Leroy’s 0xygen saturations were dropping into the 80’s, and he said he felt like he needed to go the hospital.
We all had Covid, and our son took him into the ER while I waited in the car. I had a bad cough while our son had very little symptoms. At one point in the ER, Leroy stood up and fell back. Correy caught him, and they rushed him back, thinking he was suffering a possible heart attack.
They determined he had not had a heart attack, they informed Correy, he would be admitted but it would be quite some time before a bed became available. They had started Leroy on oxygen, and he seemed to be doing better. We were told to go home, and Leroy called us when they got him into a room.
The first two and a half days, he was in a Covid unit. I was only able one time to speak with the Physician who was seeing him. I asked for Monoclonal Antibodies, and was told he could not have them because they were outpatient only. I also ask for Baricitinib. I was told it was not available. I asked for Ivermectin, and he chuckled, and told me it did nothing to help with Covid. He stated that they had started him on Remdesivir. He was doing great and would be home in a day or two. After the Dr left I went home.
Shortly thereafter, less than an hour, Leroy phoned and said they were moving him to ICU. I said, I was confused, based on the doctor’s previous comments, Leroy said they told him they could monitor him better there.
Next day, I was allowed to visit in ICCU for two hours. I immediately noticed that Leroy looked very confused as though he had no idea where he might be. On the second day, when I went to visit, I was told I could only stay a short time as they were no longer allowing any visitors to ICU.
As his condition worsened, we had no contact with him. I just wanted him to rest and get better, talking on his cell phone was difficult for him. One day was good and the next was not. I had no idea how bad he was till the day they called and said we had to have an end of life discussion.
He had never been vented, he was never put on the Bipap and only nasal canula until we were moved out of CCU for comfort care. His records indicate an acute kidney injury unspecified. No one indicated any kind of kidney issues during his entire stay.
There was one brief phone call daily about how he was. One day, I got no phone call. I called and left messages at the nurses’ station twice begging to let me come up and see him or allow me to talk with him. I cannot imagine the fear that he must have felt, or the thoughts that he must have had there by himself. The guilt of not being able to advocate or do something to be there for him will haunt our family forever. We lost a loving father, grandfather, husband, and friend to many. A baseball community lost a man who devoted time as an umpire and coach that impacted the lives of many young boys and young men.
About a week after his death, I met with a couple who were purchasing a dog kennel I was selling. I was wearing my mask and the gentlemen said he did not mean to be rude, but he wondered why I was wearing the mask. I told him because I had just lost my husband to Covid and was unsure if anyone I might run into could be at risk of getting or giving Covid. I wanted no one else to experience what we had endured. He then asked if my husband had been given Remdesivir. I thought it odd but told him, yes. He then apologized to me and said that he worked in the medical field but could not tell me for whom or where he worked. He said the Remdesivir was killing patients.
I always felt that something was never right during his stay at the hospital, especially the day that they moved him to ICU. We knew nothing about the drugs he was given. We trusted that these men and women were there to make him better. I feel like our medical system is now only driven by the amount of financial gain which can be made at the expense of all. The pain of this loss is excruciating to our entire family, and I am sure to the million plus other families in this country who have been effected by these protocols.
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please contact us at email@chbmp.org.