


Medical Information
Medical Treatment & Hospitalization
Only that they repeatedly asked us if we had been vaxxed.
It was an incompetent hospital without treatment options which lead to the death of my husband.
Activism & Follow-up
Watch & Share The Interview
Written by James (Jim) Martin
December 12, 2021
My husband, Jim, and I began having c-19 symptoms throughout the night. We coughed all during the night.
December 13, 2021 through December 22, 2021
Our symptoms progressed with fever, vomiting, diarrhea, and coughing
That mid-morning, we began the taking Ivermectin and Hydroxychloroquine.
Jim weighed approximately 215 pounds, so we thought his dosage should be around:
Ivermectin Hydroxychloroquine
20mg 200mg
I, Diane, weighed approximately 140 pounds, so we thought my dosage should be around:
Ivermectin Hydroxychloroquine
13.5mg 200mg
On day three (3), we realized we were taking the prophylaxis dosage, so we upped the dosage for the next five (5) days to:
Jim: Ivermectin Hydroxychloroquine Diane: Ivermectin Hydroxychloroquine
40mg 200mg 26mg 200mg
In addition to that, we took zinc 25 mg/day prior to getting sick
Zinc 50 mg/day
Vitamin D3 2000iu/day
Vitamin A not sure of dosage
Vitamin C 1000 mg
Plus additional nutritional supplements
Jim had hypertension, and so do I. His medications were: Eliquis, 5mg, 2x, daily; Benazepril 10 mg, hydrochlorothiazide 12.5mg, 1x daily (hospital had him taking this 2x, daily); Atenolol, 25mg, 1x, daily (hospital did not have this medication on Jim’s list of medications).
My medications were: Ramipril, 10mg, morning; Toprolol XL, 100mg, nightly.
To thwart getting pneumonia, we tried walking on our treadmill. Approximately between 12/15 and 12/19, Jim walked 3x, I walked 2x. Jim seemed to have more energy than me. He was the one taking care of me, making sure I had taken medicine, making me eat something, helping me to shower.
Thursday, December 23, 2021
Things were not getting better. By the evening of Thursday, December 23, 2021, our oxygen was in the 80s, and we both were having difficulty breathing. It was night. The urgent cares were closed. We were depending on a friend to drive us (because neither of us felt like driving), so we went to the closest facility, which was Hi-Desert Medical Center in Joshua Tree, CA. I wished we hadn’t gone there, but at the time, I thought it might be okay. After all, two close friends were there, one being our pastor. What could go wrong? (One of our sons, who works at Loma Linda University Hospital, and his wife said they would come and get us and take us to Loma Linda Hospital if we needed help, but Jim and I were afraid of giving the covid to them and their four children.)
So, we went to Hi-Desert Medical Center (HDMC) on the night of Thursday, December 23, 2021.
After the isolation screening at the hospital, which included, asking us if we were vaccinated. We were given oxygen and we were covid tested. Then we were taken to an isolation/tented area where we spent the night in a bed. The only good thing was our beds were side-by-side, and we were able to hold hands and pray together.
Medication Administered to Jim on 12/23/2021:
Time Given: 18:45 – dexamethasone dexa4i 8 mg 2 mL
18:56 – Azithromyin ns 250, 250 mL,
cefTRIAXone 1 g
21:31 – apixaban (Eliquis) 2 – 5 mg tablets (doubled his dose)
(I remember telling my husband, Jim, there must be a party going on somewhere in the hospital because the staff was gone quite a bit that night. Also, later that night, we could hear a disgruntled nurse who was complaining to another nurse regarding the gift exchange because the recipient apparently snubbed his nose at her gift.)
We were notified that we had tested positive for covid, and once there was space available, we would be moved to a room.
Blood work was done, and one of Jim’s results should have been a cause for concern since he had A-fib. His D-Dimer was 1.17, which was above the normal range. “An elevated D-dimer level suggests an increased risk of a blood clot.”1 This should have been on their radar, especially since Jim was on Eliquis because of A-fib. His labs showed CRP Quant – high, LDH / Slight Hemolysis, and Covid-19 PCR – detected.
Of course, the nurse in the isolation crew asked us if we had had the C-19 shot.
Jim received his first double dosage of apixaban (Eliquis) at 21:31.
- According to this article, a person may be at a higher risk of side effects if taking a higher dosage: https://www.healthline.com/health/drugs/eliquis-side-effects#fa-qs
“If you take too much Eliquis , call your doctor or go to the nearest hospital emergency room right away.” https://www.rxwiki.com/eliquis
Friday, December 24, 2021
Sometime in the morning, we were notified that we were going to be transferred to separate rooms. We requested to be together, which the nurse said usually didn’t happen. While the nurse went to ask if we could be kept together, we prayed to the Lord to keep us in the same room. Our prayer was answered, and we were allowed to be together – until Jim was moved to ICU.
Once getting settled in the covid isolation ward/room, the doctors and nurses asked us if we had had the C-19 shot. One doctor asked me on what basis did I make my decision, and I told him from many things we had read. (I wish I had never answered his question since it was none of his business, and he wrote my response incorrectly in his physician notes.)
Additionally, the doctor wanted us to begin a five-day regimen of Remdesivir. I questioned him, asking if there were any other options like Monoclonal antibodies available. He said remdesivir and steroidal inhaler was all this hospital offered. Then I showed him an article that reported the danger in using remdesivir for covid-19 patients. He said that was not a “real” article but a “commercial” one. He had the nurse bring out an “informational handout” about remdesivir. It definitely was not a clinical article either.
Both Jim and I refused taking Remdesivir and Baricitinib. Nursing Notes for both Jim and me on 12/24/21, by Mccall RN, Elizabeth, were reported as, “Pt refused remdesivir and baricitinib. Pt given informational handouts on drugs. Refused with verbalized understanding of risks and benefits of refusal.”
Although the nurse put down our refusal in her notes, unbeknownst to us, Jim began receiving Baricitinib from 12/24/21 through 12/31/21. I received it from 12/24/21 through 1/2/22.
Meds Administered to Jim on 12/24/2021:
Time Given: 06:02 – Iopamidol, ISOVUE-370 125 mL 85 mL
06:43 – dexamethasone, desa4i 6 mg 0.6 mL
06:49 – albuterol, albuCFC 180 mg
09:42 – famotidine (Pepcid), famo 20i 20mg 2 mL (med refused by patient)
09:43 – apixaban (Eliquis), apix2.5t 5 mg 2 tab (double dose)
Ascorbic acid (Vitamin C), 500 mg
Zinc sulfate, zinc220 220 mg 1 cap
10:45 – baricitinib, bari2t 4 mg 2 tab
12:27 – albuterol, albuCFC 180 mg
19:13 – azithromycin, ns 250 250 mL; azit 500i 500 mg 5 mL
cefTRIAXone, cert1gNS 100 add 1 g 100 mL
19:31 – albuterol, albuCFC 180 mg
19:43 – remdesivir, ns250 250 mL; remde100j 200 mg (med refused by patient)
21:34 – apixaban (Eliquis), apix2.5t 5 mg 2 tab (double dose)
21:36 – albuterol, albuCFC 180 mg
23:23 – acetaminophen (Tylenol)
enoxaparin (Lovenox), enox40i 40mg 0.4mL: From Medication Administration notes: “Med not given as per Dr. Loretto over phone.”
The nurse on duty for the morning shift, Francina Urquidez, who went by the name “France,” entered our room, according to her, and hour and a half later than she had anticipated. She told us the reason for her delay was that a patient had a problem with her aid, and it took her that long to calm down the patient. We took it in stride, but it meant our “alarm” was going off for one and a half hours, and additionally, we were connected to the IV, so we could not move much in our beds during this time.
Soon after that, another IV was attached to us by France, but this time she said to let her know when the alarm sounded and she would come and take care of it.
Well, Jim and I waited and waited for the alarm to sound, but it never did. We waited over two hours. France had apparently turned off the alarm.
After she came into the room I said I thought she could manage her time more wisely instead of arguing with patients, and that she should not have lied to me regarding the alarm; after that all hell broke loose and I never said the last thing that bothered me because she got very vocal and said, “You mean to tell me you called me in here for this when I have dying patients?!” (Her patients were not dying? We were not in ICU.) I didn’t want to argue with her. I just wanted those things brought to her attention. There was more I wanted to say, but with how angry France was, I never got the chance.
With that, my response was, “Well, that went over well.” Before leaving the room, she made sure I knew she was done with us when she curtly stated, “Don’t worry, I’ll give you your space.” After that, we never heard from her again.
Prior to contacting her, I said to my husband that I was going to talk to “France” regarding these things, and he just said, “Okay,” very softly, which now, I know, there was something wrong with him. Also during this time, I had heard him quietly weeping. It’s all very blurry because at that time, I didn’t feel good, either. Talking was difficult because of oxygen levels. Now, of course, I wish I had never brought these things up to nurse France.
In one of the texts I wrote, Jim’s oxygen level was somewhere in the 80s with the oxygen being at 100. Then other times, it was in the 90s. That’s another thing, I have tried to get his hospital records on two different occasions, and they have yet to give all of them to me. Trying to get the hospital to give all the records has been a struggle.
Saturday, December 25, 2021
At times, Jim did not seem as bad as I seemed to be. I didn’t feel like talking much; for which I am sorry for now, because I would have at least had one more conversation with him. I would have told him over and over how much I loved him. He was sitting up, texting our kids and friends and his oxygen level seemed better than mine. He told one of our friends that he was doing better than me at the time, so our friend was very surprised when he went “down hill” so quickly.
At sometime time during the day, both of us were put on full face oxygen masks.
The doctor and nurses kept pushing remdesivir, saying that people were doing better who had taken remdesivir. (They also said that they were doing better if they took it early on. Well, I didn’t think we were in the “early on” stages of having covid since our symptoms started thirteen days prior, but I felt pressured to make a decision.) I have text conversations with two of my children who were trying to help me make a decision. Finally, they both said, “Whatever you decide, Mom, we’re supporting you.”
We were asked more than once if we had been “vaccinated.” At the time, I thought we could trust the hospital staff. Now, I know we could not trust them.
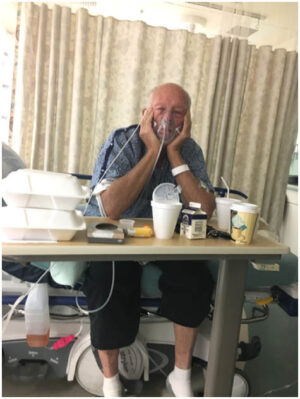
They started both of us out with the regular oxygen cannula, but soon, we were put on a larger type covering face fitting. See image of my husband, Jim. (There was no kinder and constant man than Jim. If there was or is, I have never met him. He loved and worshiped the Lord Jesus as his Savior. He loved me and told me so many times on a daily basis.)
This is the picture I took of him sometime after they told us to use those oxygen masks. He was looking at me as I took his picture.
They had both of us on a “Cardiac Diet,” which amounted to two styrofoam cups of water per day. Look how dark Jim’s urine was.
Meds Administered to Jim on 12/25/2021:
Time Given: 01:02 – albuterol, albuCFC 180 mg
04:06 – acetaminophen (Tylenol)
09:58 – apixaban (Eliquis)2 (double dose)
Ascorbic acid (Vitamin C), 500 mg 2 tab
Baricitinib, bari2t 4 mg 2tab
Dexamethasone, dexa4i 6 mg 1.5 mL
Famotidine (Pepcid), famo 20i 20 mg 2 mL
Lisinopril (Prinivil) lisi10 10 mg 1 tab
Zinc sulfate, zinc220 220 mg 1 cap
13:45 – albuterol, albuCFC 180 mg
18:24 – albuterol, albu CFC 180 mg
cefTRIAXone, cert1gNS 100 add 1g 100 mL
20:49 – apixaban (Eliquis), apix 2.5t 5 mg 2 tab (double dose)
Azithromycin, ns250 250 mL; azit500i 500mg 5 mL
Sunday, December 26, 2021
Jim was put on the BiPap at 3:30 A.M. He objected to being on the BiPap. He took a picture of himself at 5:55 A.M. with his Ipad. I was so scared for him. He kept pulling at it. The staff lied to him and said he would only be on it for three (3) hours. His heart rate (77 bpm) and oxygen levels were good.
Sometime prior to 10:12 A.M., Jim called the nurses, pulled off his BiPap mask and told them, “Choking, choking!” I was texting a friend and I said, “Between you and me am anxious. They put him on the BiPap thing. He hates it, says he is choking. They promised only a couple hours. They lied. No one to help.”
I realize now that the reason he was choking was because I suspect he was having a stroke then. After the stroke, they said he couldn’t swallow. I do know that he apparently was unable to speak, and his left side of his body was not working as well as his right side. I was hoping that they would at the very least give him a “tissue plasminogen activator, or tPA, which is a powerful clot-busting medication that can stop an ischemic stroke in its tracks.” They did not, and on the physician “Consultation Notes,” it is stated by Dr. Mohammadi on December 27, 2021, “Unclear time of onset of the patient’s symptoms, not a candidate for IV tPA as he is out of the time window for treatment.” This is pure untruth because the multiple staff came into our hospital room on the 26th and they verbally said he had a stroke. Someone did not do their job. Why did the doctor wait? The staff that was in the room (4-5 of them), knew he had a stroke on 12/26/2021. This is pure negligence.
I have been reading scriptures to Jim that we have received from texts. He seemed to like it.
11:14 A.M., I am still concerned about taking remdesivir, I asked my friend if our friend, Pat, (who was, during this same time, in the same hospital as Jim and me,) is taking remdesivir. She responded, “I think so.”
At approximately 11:41 A.M. I tell my friend that Jim is not doing well. By then, the hospital knew he had had a stroke. They had all kinds of machines hooked up, making all sorts of beeping noises with many alarms going off continuously.
Meds Administered to Jim on 12/26/2021:
00:57 – albuterol, albuCFC 180 mg
10:43 – apixaban (Eliquis, apix 2.5t 5 mg 2tab
Baricitinib, bari2t 4 mg 2 tab
Dexamethasone, dexa4i 6mg 1.5 mL
Famotidine (Pedcid), famo 20i 20 mg 2 mL
Lisinopril (Prinivil) lisi10 10 mg 1 tab
Zinc sulfate, zinc220 220 mg 1 cap
10:44 – albuterol , albuCFC 180 mg
14:43 – ascorbic acid (Vitamin C), 500 mg
17:05 – albuterol, albuCFC 180 mg
17:09 – cefTriaXone, cert1gNS 100add 1 g 100 mL
20:52 – azithromycin, ns250 250 mL; azit500i 500 mg 5 mL
hydrALAZINE hydr20i 10 mg 0.5 mL
21:00 – Apixaban (Eliquis), apix2.5t 5 mg 2 tab, (double dose) not given: 21:00 (on BiPap)
December 27, 2021
On this day, the hospital began giving Jim remdesivir. Since Jim had refused to take it on 12/24/2021, it is unclear how he began the five-day regimen, especially since I do not remember giving my permission. I was continually asked by the hospital staff for both of us to take it. I remember texting my children and asking them what we should do, but I do not remember giving the hospital permission to give it to Jim. I don’t think they had my permission to administer it to him, however, I do remember giving them permission for myself. I made this decision because the hospital made we feel like I had no other choice.
This whole remdesivir situation is making me wonder about the timing of it all. Something is amiss here. As I look back on the situation, by this time, we seemed to be doing okay – on our way to healing, so why would we need remdesivir 3-4 days into our hospital stay? What was the point of pushing to take this drug when the doctor had told me it was only effective after the early onset of covid?
Sometime during the morning, Jim was taken to ICU. As they wheeled him out, I called loudly to him, “I love you, I love you, I love you!” He wasn’t able to answer back to me. Jim never wanted us to be separated from each other. This was saddest and scariest moment in my life. I wonder if I would see my love, my soul mate ever again.
It had been four days since entering HDMC, and I had not had any of my blood pressure medications given to me. When inquiring regarding my own blood pressure medications, the nurse off-handedly said my blood pressure had been a “little low,” but is was brought to me only after my inquiry. I received first dosage of 100mg metoprolol, 12/27/21 at 20:34.
After Jim was admitted to ICU, each day, Dr. Abawi would come into my room and tell me how badly Jim was doing. He would say that he was on the BiPap machine for too long.
“How long is too long?” I asked.
He responded that he shouldn’t be on that machine for only a few hours. “He has been on it too long. It will damage his lungs. He should only be on it for a few hours.”
“What else can we do? I am desperate. I don’t want to lose my husband.” I said.
“Well, we can put him on the vent. There is always a pressure room.” Dr. Abawi replied.
“Jim doesn’t want to be put on the vent. Yes, can you see about putting him a pressure room?” I asked
“I’ll have to check into that,” was the doctor’s response. (The next day, I reminded the doctor about the “pressure oxygen tent,” but he never did anything about it.)
I was desperate for my husband to live, and I asked the doctor what we could do. He talked to me about the vent, and I said if that’s what it takes, then let’s do it. I knew it was bad news, but I was desperate for anything. Jim had voiced that he did not want the vent.
Then the doctor would ask my husband about being on the vent when Jim was in ICU. Jim would say, “No.” with the thumbs down sign. Then the doctor would come the next day and ask me again. Each day he would come in and say, “Your husband is a sick man. He has been on the BiPap for too long… His lungs can only be on the BiPap for so long.”
Then the next sentence out of his mouth would be, “Your oxygen levels are very high. You are on ‘10’.” I had no idea what that meant in medical terms. Was it bad? I didn’t know.
Repeatedly, Doctor Abawi would come in with this “news.” It was as if he didn’t know how to be a doctor. He would go in and ask my husband about being vented, then he would come to my room and ask me. Finally, on Thursday, December 30th Dr. Abawi came in to my room and said he could not vent Jim because it was against his wishes. Why didn’t he say that in the first place? He had been teetering between me and my husband when he should have known the answer all along. I was a nervous wreck knowing that Jim needed help. I felt horrible for desiring something my husband didn’t want in the first place, but I was hoping it would save him.
Once Jim had had the stroke, they (meaning the doctors and the staff) made it sound like there was no hope for him, but we did not receive a prognosis per se. No one came and spoke about what kind of stroke he had. No one came to tell us what treatment he was getting. No came to say what they had done right after the stroke. They only came to tell me how being on the BiPap was not good. That me, being on oxygen at so high a level was not good.
Meds Administered to Jim on 12/27/2021:
09:08 – dexamethasone, dexa4i 6 mg 1.5 mL
Famotidine (Pepcid), famo 20i 20 mg 2 mL
09:44 – enoxaparin (Lovenox), enox100i 98 mg 0.98 mL
11:06 – remdesivir (Veklury), ns 250 250 mL, remde100inj 200mg
17:20 – cefTRIAXone, cert1gNS 100add 1g 100 mL
20:35 – azithromycin, ns250 250 mL; azit500i 500 mg 5 mL
Enoxaparin (Lovenox), enox100i 98 mg 0.98 mL
Albuterol, albuCFC 180 mg – not given, on BiPap
December 28, 2021
After my daughter spoke with the ICU nurse around 9:30 a.m. on this day, she then sent me this text about her dad, my husband. “I wanted to make sure you saw this: Just spoke with nurse Carrie at the ICU Nurse’s station. Dad is still on the BPap but they have turned down the oxygen. His saturation level is 98%. He is responding to stimulus. He was able to nod his head in response to questions and open his eyes. He is not speaking yet, (but the nurse said that doesn’t mean he can’t, he’s just incredibly fatigued) but is moaning which is apparently a very good sign of being verbal. He is moving on his left side, his left leg has a good strength. His left arm and hand are weaker but stronger than yesterday. He does not have a catheter because of the previous situation with prostate cancer but he in is a brief and is urinating. He’s about to get his second dose of remdesivir.”
Oh, if we had only known what remdesivir would do to him.
If we were going by what the nurse said, and she was there with him more than the doctor, it appeared Jim was doing okay prior to getting remdesivir. He was responding to stimulus, able to nod his head and open his eyes. The nurse had been very encouraging about his progress.
Meds Administered to Jim on 12/28/2021:
01:00 – morphine (no ingredients listed)
02:00 to 02:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
NS 0.9% 250 mL, ns250 mL
03:00 to 03:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
04:00 to 04:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
05:00 to 05:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
06:00 to 06:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
07:00 to 07:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
08:00 to 08:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
08:10 – dexamethasone, dexa4i 6mg 1.5mL
Famotidine (Pepcid), famo 20i 20mg 2mL
08:56 – morphine, morp2i 2mg 1 mL
09:00 to 09:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
09:01 – enoxaparin (Lovenox), enox100i 98mg 0.98mL
Remdesivir (Veklury), nx250 250mL, remde100inj 100mg
09:35 – morphine (no ingredients listed)
10:00 to 10:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, 5di1000 11 mL
10:38 – D5W 1,000 mL, d5i1000 1000 mL
11:00 to 11:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 38.75 mL
12:00 to 12:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 1000 mL
13:00 to 13:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 1000 mL
14:00 to 14:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 1000 mL
15:00 to 15:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 38.75 mL
16:00 to 16:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 38.75 mL
16:46 – morphine, morp2i 2mg 1 mL
17:00 to 17:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, d5i1000 38.75 mL
17:31 – cefTRIAXone, cert1gNS 100add 1g 100mL
17:46 – morphine (no ingredients listed)
18:00 to 18:59 – NS 0.9% 250 mL, Sodium Chloride 0.9% 10 mL
D5W 1,000 mL, 5di1000 30mL
19:00 to 19:59 – D5W 1,000 mL, 5di1000 30mL
NS 0.9% 250 mL, ns250 10 mL
20:00 to 20:59 – D5W 1,000 mL, 5di1000 30mL
21:12 – azithromycin, ns250 250 mL; azit500i 500mg 5mL
enoxaparin (Lovenox), enox100i 98mg 0.98mL
21:00 to 21:59 – D5W 1,000 mL, 5di1000 30mL
22:00 to 22:59 – D5W 1,000 mL, 5di1000 30mL
23:00 to 23:59 – D5W 1,000 mL, 5di1000 30mL
Albuterol, albuCFC 180 mg, not given, on Bipap
The Physician’s Assessment Plan on this 12/28/2021, was at 15:04: “Patient’s states that he does not want to be intubated, had extensive discussion about implications of DNI. Patient comprehends and understands, and still he stated that he does not want to be intubated. Continue with high flow nasal cannula.”
Then at on same day, it stated at 15:33: “His oxygen appears to be improving as he is currently on BiPap with an FI 0.65. He will transition to high flow nasal cannula with a face mask, in addition, if needed.”
Why all of a sudden was my husband receiving morphine for pain? When was he having pain? He was moving prior to this and responding to stimuli. Why was all this medication given? Because someone moans, it doesn’t necessarily mean they are having pain. They might be trying to communicate – especially if they have lost part of that ability to speak after a stroke. On one of the reports for this day, it said “Moderate pain.” How and who would know it the pain was mild, moderate or severe if there was not communication? This is very frustrating to me.
During this time, I had remembered seeing a couple of articles where patients were lying prone to help open up their lungs. On my own, I began lying on my stomach for as many hours as I could stand it. On this day, Dr. Mohammadi came into my room and saw me lying prone. Here’s what his consultation notes stated for 12-28-2021: “The patient was encouraged to prone as much as possible, and she seemed to be quite amenable to that recommendation.” He acted as if he was the one to advise me when I was lying prone on my own.
This “recommendation” was written down on subsequent days also. Also, none of the nurses or staff recommended that I lie prone. Additionally, I began standing on my own so that I might renew my strength. I would stand by the bed for about 5 to 10 minutes per standing period. One doctor came in when I was doing my “exercise” and said not to stand too long. What that meant, I did not know.
Our children were trying to move their dad to Loma Linda University Hospital. One of our sons, knows physicians who were ready to take Jim as their patient if we got him there, but the doctors at HDMC would not release him, saying Jim might not make it there. Well, they didn’t do anything to help him here.
It was so frustrating when he was lying there and they were not doing anything but complaining about how bad he was. We trusted them, but I do not trust them now. They flubbed at the beginning by giving Jim double doses of Eliquis which can lead to brain hemorrhaging. They gave him baricitinib at the beginning, and they gave him remdesivir at the end to kill him off. Both baricitinib and remdesivir were administered against his will. I felt like they threw Jim to the dogs.
December 29, 2021
In the A.M. of this day, Dr. Abawi came into my room to tell me he did not have good news because Jim had been on the BiPap machine for four days. My text to my daughter went like this: “The doctor for Dad just came in and did not have good news. [According to the doctor] Dad has been on the machine for four days and they usually keep people on it for 24 hours. They may still have to vent him. Keep praying.”
Additionally, we had told the doctor we wanted to have Jim transferred to Loma Linda University Hospital in Loma Linda. All he kept saying was Jim was not well enough to be transferred. No encouragement at all; just negativity.
Then later in the day, my daughter had spoken to the ICU nurse and she had said, “I just sent out an update on Dad. The nurse at ICU made it sound like they are watching his lungs closely and for now he is still fine on the BiPap.”
Why would the doctor come in day-after-day and tell me my husband is doing horrible, and then the nurses would report to us such encouraging things about Jim? I felt like the doctor was a doom and gloom guy who only wanted Jim to die.
Meds Administered to Jim on 12/29/2021:
00:00 to 00:59 – D5W 1,000 mL, 5di1000 30mL
00:26 – Morphine IV additive 100mg [4 mg/hr] + NS 0.9% 100 mL, morp50120 43mg; ns100 43 mL
01:00 to 01:59 – D5W 1,000 mL, 5di1000 30mL
02:00 to 02:59 – D5W 1,000 mL, 5di1000 30mL
03:00 to 03:59 – D5W 1,000 mL, 5di1000 30mL
04:00 to 04:59 – D5W 1,000 mL, 5di1000 30mL
05:00 to 05:59 – D5W 1,000 mL, 5di1000 30mL
06:00 to 06:59 – D5W 1,000 mL, 5di1000 30mL
07:00 to 07:59 – NS 0.9% 250 mL, ns250 10 mL
08:00 to 08:59 – NS 0.9% 250 mL, ns250 10 mL
09:00 to 09:59 – NS 0.9% 250 mL, ns250 10 mL
10:00 to 10:59 – NS 0.9% 250 mL, ns250 10 mL
09:18 – Albuterol, albuCFC 180 mg*
09:19 – Albuterol, albuCFC 180 mg
09:35 – dexamethasone, dexa4i 6mg 1.5mL
Famotidine (Pepcid), famo 20i 20mg 2mL
Remdesivir (Veklury), nx250 250mL, remde100inj 100mg
10:09 – enoxaparin (Lovenox), enox100i 98mg 0.98mL
15:17 – Albuterol, albuCFC 180 mg
15:32 – morphine IV additive 100mg [4 mg/hr] + NS 0.9% 100 mL, morp50120 43mg; ns100 43 mL
16:28 – morphine (no ingredients listed)
17:03 – cefTRIAXone, cert1gNS 100add 1g 100mL
19:00 to 19:59 – D5W 1,000 mL, 5di1000 30mL
20:00 to 20:59 – D5W 1,000 mL, d5i1000 38.75 mL
21:00 – Albuterol, albuCFC 180 mg**
21:00 to 21:59 – D5W 1,000 mL, d5i1000 1000 mL
21:04 – azithromycin, ns250 250 mL; azit500i 500mg 5mL
enoxaparin (Lovenox), enox100i 98mg 0.98mL
22:00 to 22:59 – D5W 1,000 mL, d5i1000 1000 mL
22:23 – morphine, morp2i 2mg 1 mL
23:00 to 23:59 – D5W 1,000 mL, 5di1000 30mL
23:00 – morphine (no ingredients listed)***
*Ordered on previous shift, not documented that it was done.
**Not given; patient unable to follow direction.
So, Jim was able to receive Albuterol, which is a steroidal inhailer? How he was able to inhale during this time is beyond me. He was on the BiPap.
***Why is this dosage of morphine given so closely to the previous dose?
(Morphine, morp2i2mg 1 mL, given at: 22:23
Morphine, (no ingredients listed), given at: 23:00)
Of course, none of our family nor I were permitted to visit Jim the entire time he was in ICU. He was all alone.
December 30, 2021
Meds Administered to Jim on 12/30/2021:
01:00 – Albuterol, albuCFC 180 mg
01:00 to 01:59 – D5W 1,000 mL, 5di1000 30mL
D5W 1,000 mL, d5i1000 38.75 mL
02:00 to 02:59 – D5W 1,000 mL, d5i1000 38.75 mL
03:00 to 03:59 – D5W 1,000 mL, d5i1000 1000 mL
04:00 to 04:59 – D5W 1,000 mL, d5i1000 1000 mL
05:00 to 05:59 – D5W 1,000 mL, d5i1000 38.75 mL
06:00 to 06:59 – D5W 1,000 mL, d5i1000 1000 mL
08:20 – Albuterol, albuCFC 180 mg
08:46 – dexamethasone, dexa4i 6mg 1.5mL
enoxaparin (Lovenox), enox100i 98mg 0.98mL
Famotidine (Pepcid), famo 20i 20mg 2mL
09:23 – Remdesivir (Veklury), nx250 250mL, remde100inj 100mg
13:00 to 13:59 – D5W 1,000 mL, d5i1000 38.75 mL
13:29 – D5W 1,000 mL, d5i1000 1000 mL
14:00 to 14:59 – D5W 1,000 mL, 5di1000 75 mL
14:55 – Morphine (no ingredients listed),
15:15 – LORazepam (Ativan), lora2i 1mg 0.5 mL
18:23 – Morphine IV additive 100mg [4 mg/hr], morp2i 2mg 1 mL
18:37 – cefTRIAXone, cert1gNS 100add 1g 100mL
18:45 – LORazepam (Ativan), lora2i 1mg 0.5 mL
19:00 to 19:59 – D5W 1,000 mL, 5di1000 75 mL
20:00 to 20:59 – D5W 1,000 mL, 5di1000 75 mL
20:40 – Morphine (no ingredients listed),
21:00 – Azithromycin, ns250 250 mL; azit500i 500mg 5mL
enoxaparin (Lovenox), enox100i 98mg 0.98mL
21:00 to 21:59 – D5W 1,000 mL, 5di1000 75 mL
22:00 to 22:59 – D5W 1,000 mL, 5di1000 75 mL
22:09 – Morphine, morp2i 2mg 1 mL
23:00 to 23:59 – D5W 1,000 mL, 5di1000 75 mL
Finally, on this day, my daughter and son were able to arrange for me to see Jim. The reason being for the visit to see him, was they didn’t think he was going to make it. The doctor had asked our family if we wanted Jim to continue on the BiPap machine. This was heart wrenching. Why was this doctor pushing for my husband to be taken off the BiPap. What was so important to Dr. Abawi that he should come to us (my children and myself) and push for us to make a decision about my Jim’s life? Jim could still communicate. The doctor told us he was able to communicate by using a “thumbs up” or “thumps down” motion. Why did we need to take him off these machines if he was able to live? Who were we that we choose to take away his life? Dr. Abawi came at me with an urgency, and it made me think a decision must be made soon when Jim might have been healing. Who was to know? If only he hadn’t pushed us to think Jim was not doing well.
I was desperate for my husband to live, and I asked the doctor what we could do. He talked to me about the vent, and I said if that’s what it takes, then let’s do it. I knew it was bad news, but I was desperate for anything. Then the doctor would ask my husband in ICU about being on the vent. Jim would say, “No.” with the thumbs down sign. Then the doctor would come the next day and ask me again. Each day he would come in and say, “Your husband is a sick man. He has been on the BiPap for too long… His lungs can only be on the BiPap for so long.”
Right after telling me about Jim being on the BiPap, he’d say to me, “Your oxygen levels are very high. You are on ‘10’.” I had no idea what that meant in medical terms. Was it bad? I didn’t know. Repeatedly, Doctor Abawi would come in with this “news.” It was as if he didn’t know how to be a doctor. He would go in and ask my husband about being vented, then he would come to my room and ask me.
Finally, on Thursday, December 30th Dr. Abawi came in to my room during the day, and said he could not vent Jim because it was against his wishes. Why didn’t he say that in the first place? He had been teetering between me and my husband when she should have known the answer all along. I felt horrible for desiring something my husband didn’t want in the first place, but on the other hand, I was hoping it would save him.
At approximately, 7:30 P.M., I was wheeled into the ICU to see Jim. Because we had decided he would be taken off the BiPap, I was able to see him and visit with him.
What a gruesome area they had for covid19 ICU patients. As I recall, it was a large room with three tented areas, and the tented area was darker inside than the general room. That was where my Jim was placed – inside one of these large tented areas.
I was right next to his bed, and I held his hand, and I read to him some things I had written earlier about our life together as a wonderful son, husband, father, friend and worshiper of Christ. After reading, I heard a whimper from him and I mentioned it to the nurse who happened into the tent. She said, “That was just a grunt.” I thought she was nuts, but I didn’t say anything because I wanted to keep the situation calm. My initial reaction was, “I know my husband better than you. We’ve been married over 51 years.” It’s these kinds of comments I did not appreciate from the medical staff.
Our children FaceTimed with me and they got to see and talk to their dad during the call. It was wonderful to hear all four children telling their father they loved him, and telling him they would take care of me. At the same time, I was heartbroken and I couldn’t believe this was happening to our family. We were torn apart when they killed Jim. These adult kids still asked their dad for advice on matters, and they would call and have wonderful conversations with him.
All throughout his life, Jim loved worshiping the Lord in praise and with songs. I had brought in my Kindle and we played Christian music for him. Once he heard it, he lifted his right hand and he began waving his arm to the beat of the music. If Jim was capable of hearing the music and responding to it, why did the doctor think he was on death’s door. I felt like we were killing him.
After about an hour, I was tiring, so I asked to be taken back to my room. If I had been thinking better, I would have had Jim move over a bit (or had the nurse move him over to the side of the bed), and I would have hopped in bed with him and lain by his side. If only.
By now, Jim had been on remdesivir for four days.
December 31, 2021
Meds Administered to Jim on 12/31/2021, the day of Jim’s passing:
00:00 to 00:59 – D5W 1,000 mL, 5di1000 75 mL
00:09 – LORazepam (Ativan), lora2i 1mg 0.5 mL
00:40 – LORazepam (Ativan), lora2i 1mg 0.5 mL
01:00 to 01:59 – D5W 1,000 mL, 5di1000 75 mL
01:58 – Morphine, morp4i 4mg 1 mL
02:00 to 02:59 – D5W 1,000 mL, 5di1000 75 mL
02:30 – Morphine (no ingredients listed)
03:00 to 03:59 – D5W 1,000 mL, 5di1000 75 mL
04:00 to 04:59 – D5W 1,000 mL, 5di1000 75 mL
05:00 to 05:59 – D5W 1,000 mL, 5di1000 75 mL
05:20 – Morphine, morp4i 4mg 1 mL
06:00 to 06:59 – D5W 1,000 mL, 5di1000 75 mL
07:00 to 07:59 – D5W 1,000 mL, 5di1000 75 mL
08:00 to 08:59 – D5W 1,000 mL, 5di1000 75 mL
08:36 – dexamethasone, dexa4i 6mg 1.5mL
Famotidine (Pepcid), famo 20i 20mg 2mL
08:39 – enoxaparin (Lovenox), enox100i 98mg 0.98mL
08:54 – remdesivir (Veklury), nx250 250mL, remde100inj 100mg*
09:00 to 09:59 – D5W 1,000 mL, 5di1000 75 mL
10:00 to 10:59 – D5W 1,000 mL, 5di1000 75 mL
11:00 to 11:59 – D5W 1,000 mL, 5di1000 75 mL
11:29 – Morphine (no ingredients listed)
14:04 – Morphine IV additive 100 mg [4 mg/hr], morp50i20 100 mg 2 mL 4mg/hr; ns 100 100 mL
14:15 – Morphine IV additive 100 mg [4mg/hr] + NS 0.9% 100 mL, morp50i20 5 mg/hr
14:30 – Morphine IV additive 100 mg [4 mg/hr] + NS 0.9% 100 mL, morp50i20 6mg/hr
14:59 – Morphine IV additive 100mg [4 mg/hr] + NS 0.9% 100 mL, morp50i20 43 mg; ns100 443 mL
14:45 – Morphine IV additive 100 mg [4 mg/hr] +NS 0.9% 100 mL, morp 50i20 7 mg/hr
15:50 – LORazepam (Ativan), lora2i 1mg 0.5 mL
*Of course, Jim had to receive his last dosage of remdesivir to make sure it was documented that he got the five dosages. The hospital probably would not have received their incentive if hadn’t been given the full dosage amount of five days.
Once we entered the room, the nurse immediately took off the BiPap – almost as if she ripped it off. If I had known what was happening, I would have asked her to leave it on for a while so we could talk, pray and be with Jim longer before he left. Those precious moments were ripped right out from us.
He was breathing a bit on his own, but not for long. Our family was singing hymns, praying, loving on their dad by saying their good-byes and telling him we loved him. I was hugging and kissing my precious man into eternity and telling him I loved him.
My beautiful husband passed on Friday, December 31, 2021, at 2:45 P.M., with his family surrounding him in love and prayers.
January 1, 2022
Dr. Abawi came into my room, and he continued in an accusatory tone that I was still on high oxygen. Finally, I got the nerve to answer back with, “What do you want me to do?” because honestly, I had no idea. My husband has just passed away, and he acted like it was my fault that I was still at a number “10” oxygen setting. I am not a medical professional, and I did not know what I should be doing about this situation. For the past few days I had been applying my own medical therapy by lying prone while resting and sleeping, and by standing by the hospital bed several times a day.
Right then, the doctor angrily said to the nurse who was in the room at the time, “Turn down that oxygen to seven (7)!”
Well, that really scared me because I didn’t know if I would be able tolerate such a sudden switch to a lower oxygen level.
An hour passed, and I was able to tolerate the lower level. Again, suddenly, the staff came into the room and lowered my oxygen to a number four (4). Now my anxiety was high. No explanation. Not, “We are going to lower you oxygen level to a four, Diane. Are you okay with that?” They just came into the room and turned it down.
Wow! How amazed they must have been when they realized I could tolerate being that low on the oxygen flow.
My question was, why hadn’t that tried it or made notice of it prior to that? I’ll tell you. It was negligence on their part. They weren’t paying any attention to me, and how to get me on the path to healing. Their way of treating covid was to give patients drugs – baricitinib, cefTRIAXone, dexamethasone, enoxaparin (Lovenox), lopamidol and remdesivir.
Oh, and I want to say, that my son had to call the hospital a few times to ensure that I had the proper meals. Several times, I received meals two or three hours later. One “breakfast,” I received what we had been given the previous evening for dinner.
January 2, 2022
After surviving remdesivir and baricitinib, I was sent home from the hospital with oxygen on this date.
Sincerely,
Diane Martin
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please contact us at email@chbmp.org.
